Posted August 05, 2025 in Fertility Blog & Information
15 minute read
Key Takeaways
- Endometriomas impact fertility by compromising ovarian function, egg quality, and hormonal balance, causing conception to be a struggle for countless women across the globe.
- While the surgical removal of endometriomas can improve pregnancy rates, it can impact the available ovarian reserve, highlighting the importance of careful surgical planning and technique.
- The size and characteristics of the cyst, patient age and ovarian reserve play a role in predicting fertility after surgery.
- Post-op care — such as consistent follow-up and lifestyle tweaks — are essential for facilitating recovery and maximizing reproductive health.
- Fertility treatments like assisted reproductive technologies might be advised to improve pregnancy chances post-surgery, particularly if natural conception proves challenging.
- Open dialogue with doctors and including partners in the process can assist women in addressing the emotional and medical challenges of endometrioma surgery and baby chances.
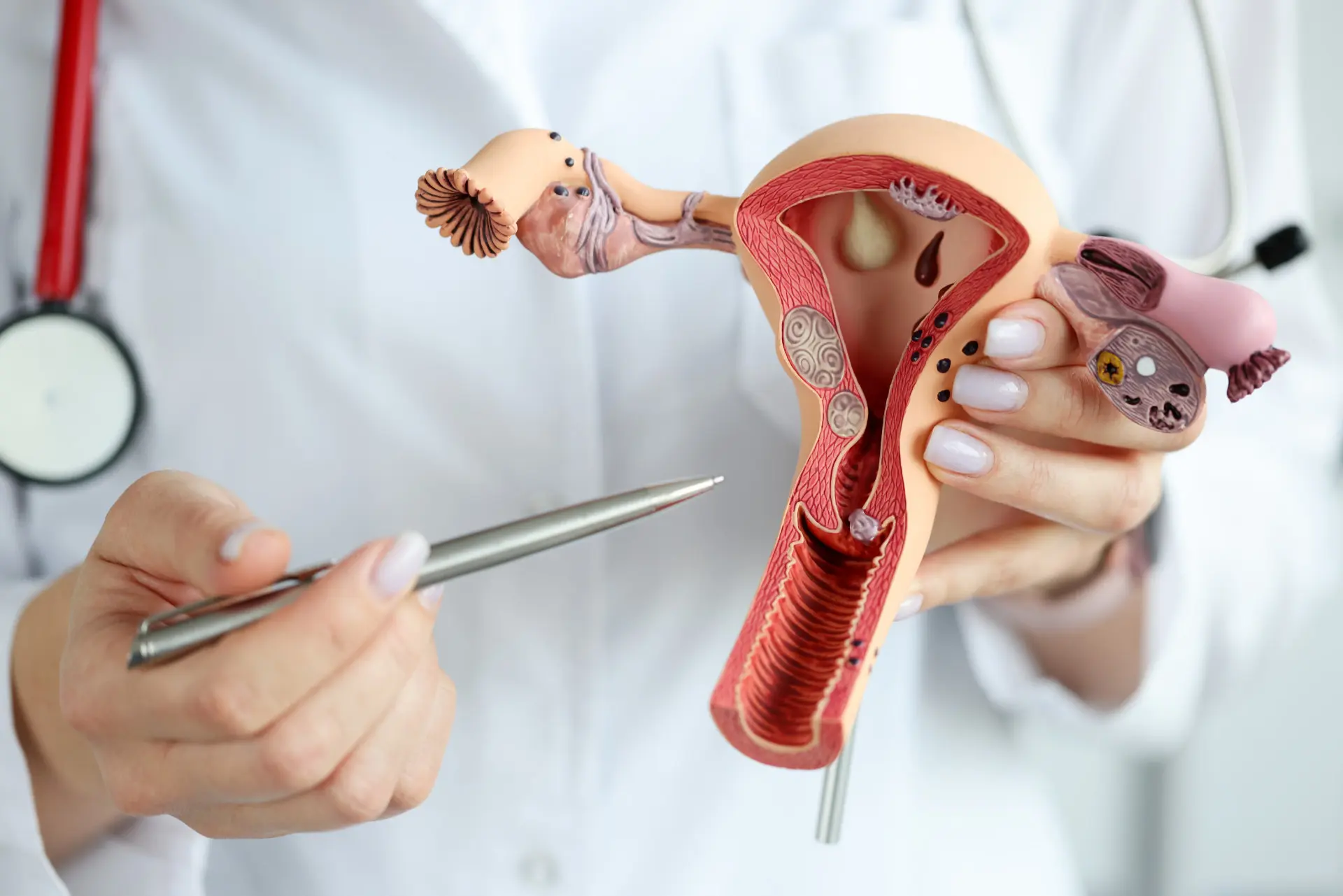
How endometrioma surgery can impact baby making odds of individuals with endometriosis-induced ovarian cysts. Surgeons commonly excise these cysts to relieve pain or increase natural pregnancy chances. Other studies demonstrate higher pregnancy rates following surgery, but these can be related to cyst size, type of surgery, and age. They check ovarian reserve both prior to and after the procedure so that they can monitor the effect it has on one’s egg supply. Recovery time and risks, like scar tissue, can impact baby chances post surgery. Every situation is unique and requires guidance from your physician. The main body will discuss surgery options, what studies say about fertility, and advice on planning for a family after endometrioma surgery.
The Fertility Dilemma
Endometriomas, or ovarian cysts caused by endometriosis, may alter the route to conception in multiple ways. Their presence is frequently problematic when it comes to fertility. Here’s how endometriomas can affect baby chances:
- Endometriomas can reduce ovarian reserve, evidenced by diminished anti-Müllerian hormone (AMH) levels. That translates into less eggs available for fertilization.
- Large cysts can destroy adjacent healthy tissue, exerting toxic effects that impair ovarian function and egg quality.
- Even mild, chronic inflammation stemming from endometriosis can hurt hormone balance and disrupt egg development.
- Surgery excises cysts but can decrease egg count, particularly if healthy ovary tissue is sacrificed.
- How much an endometrioma affects egg quality depends on how large it is—the larger the cyst, the more likely it is to be detrimental.
- Endometrioma women may yield less eggs – particularly from the affected ovary.
- Spontaneous pregnancy rates decrease by approximately 15% post-surgery versus those who proceed directly to IVF.
- Cyst presence can make pregnancy less predictable.
- Endometriomas carry an extremely low risk of infection or contamination during IVF, and therefore they do not warrant surgery just for IVF preparation.
- Or surgical pretreatment doesn’t necessarily increase chance of live birth and freeze-all strategies frequently demonstrate superior outcomes compared to fresh transfer.
Cyst Environment
The intra-endometrioma environment is not ovarian friendly. Inflammation triggered by the cyst can disrupt local hormonal milieu and destroy oocytes. This makes it difficult for the ovary to function properly. Too often, healthy tissue gets injured, cutting ovarian reserve and wrecking fertility. Doctors monitor cyst size, shape and growth in order to assist with fertility plan decisions.
Ovarian Function
Endometriomas can disrupt ovarian function and the ovary’s hormone response. Surgery may recover function if cysts are large or painful but can damage the ovary if too much tissue is removed. Normal ovulation can cease or become erratic from both the cyst and surgery. It’s crucial to preserve as much healthy ovarian tissue as possible with surgery, so that future fertility prospects remain greater.
Egg Quality
Endometriosis lesions—particularly endometriomas—can reduce egg quality by inducing stress and inflammation in the ovary. Research reveals women with these cysts tend to have decreased markers of ovarian reserve, such as AMH, and decreased numbers of high-quality eggs. Post surgery, egg quality can rebound if inflammation decreases, but it’s individual. These hormonal treatments are occasionally administered to enhance egg quality prior to fertility treatments, and physicians might recommend them depending on individual cases.
Surgical Impact
Endometrioma surgery alters future fertility in numerous respects. The surgery, the tumor burden, the surgeon’s expertise, all count. Age and other conditions, such as adenomyosis, can influence results. This part dissects how surgery can help or harm baby odds.
1. Ovarian Reserve
Endometrioma surgery can decrease ovarian reserve — fewer eggs remain after surgical intervention. This is a ticking time bomb for women over 35, since age alone already reduces egg number. Doctors measure ovarian reserve pre- and post-surgery with markers such as anti-Müllerian hormone (AMH) and antral follicle count. These tests assist in anticipating how the ovaries may react to treatment down the road.
Some women regain ovarian reserve if a small cyst is excised, but those with large/bilateral cysts or stage IV disease typically experience a more significant AMH decline at 1 year. When ovarian reserve is low, it’s harder to conceive naturally and IVF may be required, although success rates can decline too.
2. Cyst Removal
Complete cyst removal is important for fertility. Research demonstrates improved pregnancy rates following complete excision of endometriosis deposits (68.5%) as compared to partial excision (41.7%). Laparoscopy is less invasive and typically has a quicker recovery than an open surgery (laparotomy), but both types of procedures target complete cyst removal. If some cyst tissue remains, pain and endometriosis can return, reducing fertility.
Removing the cyst can relieve symptoms such as pelvic pain and enhance ovarian function, supporting reproductive health.
3. Surgical Technique
Surgical impact molds immediate and long-term fertility as well. Laparoscopy, a minimally-invasive approach, preserves more ovarian tissue and reduces risks of scarring. Meticulous work in the operating room reduces complications, such as infection or bleeding, that can impact fertility. The technique decision impacts healing time and how quick women can attempt conception. Overzealous surgery will zap good tissue, damaging fertility, while saving too little risks leaving disease. Striking the balance between aggressive disease clearance and conservation of tissue is the equation for good outcomes all around.
4. Natural Conception
Natural conception is achievable following endometrioma surgery, particularly when ovarian reserve remains robust. Peak pregnancy rates are 3–6 months post surgery. Younger women and full cyst removal have higher chances. Ovulation tracking and timing intercourse during fertile windows assist. Healthy lifestyle—good diet, no smoking, moderate exercise—can increase the odds.
5. IVF Outcomes
Previous endometrioma surgery may influence IVF outcomes. Reduced ovarian reserve post-surgery can translate to diminished eggs for IVF. Excising cysts can sometimes make the ovaries more accessible at egg retrieval. The method of surgery, such as laparoscopy, may assist in maintaining egg quality. Individualized IVF strategies, factoring in age, AMH, and surgical history, produce optimal outcomes.
Predicting Success
Knowledge that can help you predict your success Every patient presents differently and we make our best predictions based on age, cyst characteristics and pre-operative testing.
Patient Age
Age is the single most significant factor in women with endometriomas who desire pregnancy. As women age, the quantity and quality of their eggs diminishes. This decline can accelerate in those with endometriosis. Younger endometrioma patients tend to have superior ovarian reserve, thus more eggs post-surgery. For instance, women who are under 35 frequently exhibit better post-surgical pregnancy rates than those over 40.
Early action is essential for younger females. Chances of a successful live birth after surgery decline with age. Research indicates the live birth rate a year after laparoscopy is around 52%, though it’s higher for women in their early 30s or younger. Women older than 38 might get lower chances, even with surgery and fertility treatments.
Cyst Characteristics
The size and type of cysts make a difference in forecasting fertility. Big endometriomas, typically > 4 cm, can damage healthy ovarian tissue. Multiple or bilateral cysts may compromise the ovarian reserve to a greater extent than a single small cyst. Imaging studies such as ultrasound or MRI allow physicians to visualize the number, size, and location of cysts preoperatively and thereby inform surgical planning.
Cyst features influence the risk of recurrence as well. Larger or complex cysts tend to have a higher probability of returning, potentially reducing the likelihood of pregnancy later on. If cysts are deep or impact both ovaries, this can help inform physicians to recommend alternative fertility options, like assisted reproductive technology. These characteristics are factors in surgical planning and conversations about future pregnancy likelihood.
Pre-Surgery Tests
Tests done before surgery help doctors know if a woman still has enough eggs and how well her ovaries work. Blood tests for hormones like AMH (anti-Müllerian hormone) or FSH (follicle-stimulating hormone) show ovarian reserve. Imaging, especially transvaginal ultrasound, looks at cysts and ovarian tissue.
Hormone results and imaging both identify issues that could reduce the chances of pregnancy post-surgery. These tests are crucial for crafting a personal plan. For instance, low AMH or many cysts might make earlier use of IVF the smarter option. These steps both establish real expectations and direct therapy.
Beyond The Scalpel
Endometrioma surgery is just one step in patients’ family-building journeys. What you do after surgery counts just as much as what happens in the operating room. A combination of post-op care, lifestyle changes and medical assistance determines each patient’s odds. Continued coaching keeps you on target and your questions at the forefront.
Post-Op Care
Post-operative care is crucial for fertility preservation following endometrioma surgery. As many as 20% of patients will be infertile from pelvic adhesions so they need to be very carefully managed. Early identification of issues such as infection or hemorrhage is crucial. Intraoperative bleeding of less than 50 ml is associated with increased pregnancy and live birth rates within 12 months after surgery. Regular follow-ups enable early intervention in case new symptoms appear or recovery is slower than anticipated.
- Key components of post-op care: * Care of wounds and hygiene
- Pain control
- Observe for infection or fever
- Keeping tabs on periods
- Restricting heavy activity
- Observing any abnormal pain or drainage
- Attending all follow-up appointments
Follow-up visits provide providers an opportunity to monitor healing, go over reproductive goals, and talk next steps for those who are planning pregnancy.
Lifestyle Adjustments
- Eat a well-balanced diet with plenty of fruits, vegetables, lean proteins.
- Engage in moderate exercise such as walking or swimming
- Avoid tobacco, excessive alcohol, and recreational drugs
- Manage stress with yoga, meditation, or counseling
- Aim for regular sleep patterns
Smart nutrition and restorative movement can help nurture hormonal health and healing. It controls weight, which too can influence fertility outcomes. Such stress reduction strategies as meditation help keep menstrual cycles in check and may even boost fertility. Abstaining from toxins is associated with improved reproductive health across the ages.
Fertility Treatments
Fertility meds might ramp up ovarian response post-surgery, particularly where ovarian reserve is diminished. Personalized treatment plans consider patient age, AMH levels, and time attempting. Assisted reproductive technologies—such as IVF—provide an alternative route, especially for older women (35+) or those with diminished AMH. Treatments can collaborate with surgery to increase the success rates, as the cumulative pregnancy rate increases from 14.6% at three months to 57.3% at one year after surgery.
Monitoring and Support
Follow up monitors changes in hormone levels and ovarian function. A little early help can catch problems before they impact fertility. Age and AMH are the better outcome predictors. Other pieces of advice and communication that help the patient timely informed decision making.
The Recurrence Question
Endometrioma recurrence is frequent and highly variable after surgery, which is a real issue for those wishing to conceive. Recurrence rates vary from 6% to 67% at 5 years, and this broad spectrum demonstrates the unpredictability post-surgery. It’s riskier for more severe endometriosis. In stage III, 22.6% of patients experienced recurrence, and 20.3% did in stage IV. Even when moderate to severe endo lesions are excised, recurrence can be as high as 67%. The stage and how much of the disease is resected both come into play.
| Factor | How It Adds to Recurrence |
|---|---|
| Stage of endometriosis | Higher stages mean higher recurrence risk |
| Completeness of surgery | Leftover lesions can grow back |
| Post-op medication | Can lower risk, but not always by much |
| Hormonal environment | Changes can restart lesion growth |
| Patient age | Younger age linked with higher recurrence |
| Genetic background | May affect body’s response after surgery |
Recurrence can damage pregnancy odds. When endometriomas recur, they can harm the ovaries or inhibit egg maturation. This decreases the chance of conceiving, whether one is trying naturally or with assistance from treatments such as IVF. Sometimes, that recurrence cysts means more surgery, which can additionally lower ovarian reserve. It becomes a recurrence question that can each time impact your fertility and your window to conceive.
To assist in reducing this risk, physicians commonly recommend periodic checkups and imaging to identify early symptoms of new cysts. Post-surgical hormone therapies may assist, yet they’re not effective for all individuals. Some women experience recurrence even with medicine — in one study, 27.4% of those who took medicine had recurrence, versus 16% who received no additional treatment. Surgical technique is important. Completely removing all visible lesions reduces the chances, but occasionally small fragments are left behind and can regrow.
Navigating The Grey Zone
Endometrioma surgery and pregnancy hopes is not a direct line. They are frequently difficult decisions, influenced by medical realities, individual ethics, and the desperation of infertility. Both surgery and waiting, for each step has its own mutation of risks and hopes.
The “Watchful Waiting” Path
Some women might decide to delay surgery, a decision referred to as “watchful waiting.” That is, monitoring cysts with scans rather than immediately excising them.
This route can reduce the risk of surgical damage to the ovaries. Waiting doesn’t keep pain away or cysts at bay. Periodic monitoring is required to determine if the cyst transforms in form, dimensions or induces novel discomfort. If a cyst grows beyond 4–5 cm, impacts fertility or causes harsh symptoms, surgery could be in order.
Other alternatives are hormone therapy. Some women take birth control pills, progestins or GnRH agonists to slow cyst growth. These therapies may not be appropriate for all people, particularly those attempting to conceive. Each plan should suit the person’s objectives and well-being.
The Emotional Toll
Endometriosis can be isolating and exhausting. Women are stressful or sad or guilty when it’s hard to conceive.
Mental health assistance is critical. A good counselor can provide strategies to manage grief, rage, or anxiety. Support groups can provide both comfort and real-life accounts from others in the same boat.
Partners go a long way, as well. A quick chat or a walk together can lighten difficult days.
A Partnered Decision
Assists when partners hop on the surgery and baby planning discussions. Sharing decisions can create trust and get both parties on the same team.
Candid discussion of concerns, aspirations and immediate plans keeps all parties transparent. This shared strategy frequently provides peace of mind, allowing you to better confront disappointments or select new alternatives.
A support bond can lighten the burden of endometriosis and infertility — even when the path ahead is unknown.
Conclusion
Endometrioma surgery can assist certain individuals in getting pregnant, but it doesn’t provide a guarantee. Physicians consider age, ovarian reserve, and previous health to assist direct decisions. Surgery may relieve pain and increase fertility for some, but it can reduce ovarian reserve and is not without risks. It recurs frequently, so follow-up remains essential. Many do best with a combination of care–surgery, medications, and occasionally IVF. Maintain open communication with your care team. Ask questions, share your hopes, be engaged at every step. Each case looks slightly different. For more information or assistance, contact a trusted physician or fertility clinic. Your journey counts—advance with great information and support.
Frequently Asked Questions
Can endometrioma surgery improve fertility?
Yes, endometrioma surgery can increase your baby odds, particularly for women experiencing pain or those with large cysts. Ave, results differ. Others will require fertility assistance post surgery.
Does endometrioma surgery reduce ovarian reserve?
Surgery can reduce ovarian reserve by excising normal tissue as well as the cyst. The risk is contingent upon the endometrioma’s size, location, and the surgical technique employed.
How soon after endometrioma surgery can I try to conceive?
Most doctors suggest waiting 2-3 months post surgery before trying to get pregnant. This gives your body time to recover and lessens the possibility of complications.
What are the chances of pregnancy after endometrioma surgery?
Pregnancy rates post-surgery differ, but research indicates approximately 30% to 50% of women could become pregnant naturally within a year. Your personal chances depend on age, ovarian reserve, and other considerations.
Can endometriomas come back after surgery?
Yes, endometriomas can recur post surgery. Recurrence rates are 20-50% by the five years. Consistent tracking and check-in with a doctor is key.
Is IVF recommended after endometrioma surgery?
IVF might be advised if natural conception does not take place or in the presence of additional fertility problems. IVF success rates can be comparable to those in women without endometriomas, based on age and ovarian reserve.
Are there risks to the baby if conceived after endometrioma surgery?
To risk for birth defects or complications for babies conceived following endometrioma surgery. Preconception counseling can assist with any particular issues.
