Posted February 04, 2026 in Fertility Blog & Information
17 minute read
Key Takeaways
- Diminished ovarian reserve implies that fewer and often lower-quality eggs are left, thereby shortening your reproductive window and potentially limiting success with fertility treatments. Think early testing and preserving options.
- Key diagnostic tools include AMH, FSH, estradiol blood tests, and transvaginal ultrasound antral follicle counts. Clinicians combine these results to tailor treatment recommendations.
- Your options range from trying with your own eggs using personalized stimulation protocols to donor eggs or embryo adoption. Look back at previous stimulation responses and talk realistic success rates with your clinician.
- Lifestyle measures including a balanced, antioxidant-rich diet, achieving and maintaining a healthy weight, avoiding smoking and excess alcohol, and taking recommended supplements can complement medical care to support overall reproductive health.
- Emotional support is key. Seek counseling, support groups, and bring partners or trusted family through grief, stress, and decision making during diagnosis and treatment.
- What you can do now — track cycles, schedule ovarian reserve testing, document medical and family history, and create a reproductive timeline to help inform next steps and treatment planning.
Diminished ovarian reserve means a reduced quantity and quality of your eggs. It frequently manifests as reduced AMH, reduced follicles on ultrasound or accelerated egg loss with age.
Causes include genetics, surgery, medical treatment, or unknown factors. The remainder of this post breaks down the tests, timelines, and options for family building and fertility care related to diminished ovarian reserve.
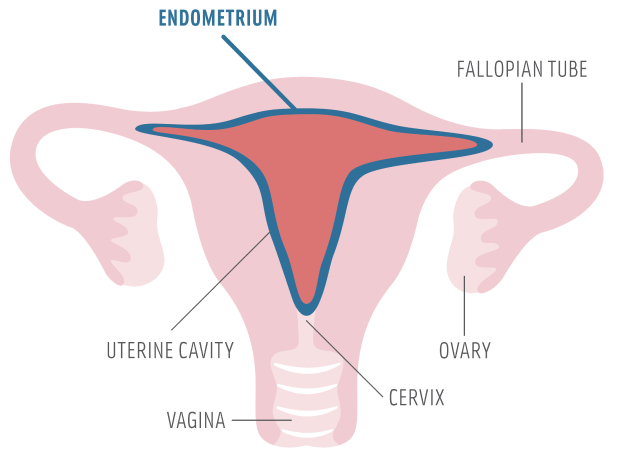
Understanding Ovarian Reserve
About ovarian reserve – the number and quality of eggs remaining. It establishes the baseline for natural fertility and for response to assisted reproduction. There isn’t a single uniform definition of reserve, but tests like anti-müllerian hormone (AMH), antral follicle count (AFC), and basal follicle-stimulating hormone (FSH) are used to estimate reserve.
AMH and AFC tend to be the best indicators, but FSH and estradiol provide additional insights into cycle-day hormone balance. Diminished ovarian reserve (DOR) can be caused by age, genetics, medical treatments, environmental exposures, or past ovarian surgery. It can present at any age, but frequently becomes more apparent after the age of 30.
1. Egg Quantity
Egg count declines with age in a steady and accelerating pattern. Loss can be evident by age 30 and accelerates over the next decade. Antral follicle count on transvaginal ultrasound and AMH levels in serum serve as key markers of this quantity.
Low egg quantity means fewer recruitable follicles in a cycle and fewer mature oocytes at retrieval during IVF. Examples: a typical AFC of 10 to 15 and AMH of 2 to 4 ng/mL suggest good reserve. An AFC less than 7 and AMH less than 1 ng/mL often signals diminished reserve.
2. Egg Quality
Egg quality declines with age, increasing the likelihood of chromosomal abnormalities in embryos and higher miscarriage risk. Poor egg quality manifests in reduced live birth rates per cycle even when eggs are retrieved.
Diminished Ovarian Reserve often overlaps with diminished egg quality, but the two are not synonymous. Younger individuals can have low quantity but relatively preserved quality in some scenarios. Embryo viability depends not only on the quantity of eggs but also on genetic quality, so egg quality is critical for a healthy pregnancy.
3. Key Hormones
AMH, FSH and estradiol are primary markers. High basal FSH or low AMH are very suggestive of diminished reserve. Estradiol can suppress FSH if measured late in the follicular phase.
Hormone shifts alter cycle regularity and ovulation predictability, generating abbreviated cycles or inconsistent ovulation timing. Normal versus abnormal cutoffs differ by lab, but practical cutoffs applied in clinical care include AMH less than 1 ng/mL and FSH greater than 10 to 12 IU/L as red flags prompting additional work-up.
4. Your Timeline
DOR abbreviates the fertile window and can put a timing crunch on planning. Monitor your cycles and ovulation symptoms for early warnings. A shorter cycle or missed ovulation can indicate change.
Perimenopause hastens the decline, and approximately 1% of individuals undergo menopause before the age of 40, which is known as premature ovarian failure. Create a rough timeline that couples age, ovarian tests, and your goals for deciding whether to conceive, preserve, or treat.
Causes and Risks
Diminished ovarian reserve is a consequence of a combination of biological, genetic, medical, and environmental causes. Knowing these causes helps explain who is at risk, why age is important, and what can be modified when designing fertility care.
Age
Increasing maternal age is the primary cause of DOR. After roughly age 35, both the rate of follicle loss and the decrease in egg quality become even more rapid. This decrease increases the risk of a bad response to stimulation, lower success with natural conception, and earlier menopause in certain women.
Age affects egg number and egg quality: fewer eggs remain and the eggs that do remain are more likely to carry chromosomal errors that reduce implantation and increase miscarriage risk.
Genetics
Genetic causes can directly deplete ovarian reserve. Fragile X premutation carriers and chromosomal abnormalities are established causes of POI. A family history of early menopause or premature ovarian failure means higher personal risk and typically indicates inherited factors that reduce the length of reproductive life.
Other gene variants, still being researched, could affect the rate at which the ovarian pool exhausts. Fragile X-associated primary ovarian insufficiency, Turner syndrome and mosaicism, and specific X-chromosome deletions are the genetic disorders with low ovarian reserve.
Medical History
Historical events and medical treatments can significantly alter ovarian function. Ovarian surgery, particularly cystectomy or partial oophorectomy, can deplete egg reserve. Pelvic radiation and alkylating agents are highly toxic to ovarian tissue and commonly induce permanent damage.
Autoimmune diseases and untreated thyroid disorders can disrupt normal ovarian signaling. Endometriosis and pelvic inflammatory disease can damage ovarian tissue directly or through inflammation, while PCOS shifts hormonal balance in patterns that can impair oocyte development. A complete medical history is essential in evaluating infertility and care planning.
Environment
Environmental and lifestyle exposures mold ovarian health throughout life. Smoking depletes follicle loss and reduces ovarian reserve, while heavy alcohol consumption is correlated with detrimental outcomes. Pesticides, heavy metals like lead and cadmium, and some industrial chemicals correlate with lower reserve in studies.
Some drugs and chronic workplace exposures contribute risk. Maternal nutrition matters too: undernutrition or an obesogenic maternal diet can reduce offspring ovarian reserve.
Checklist of environmental risk factors with brief notes:
- Smoking: direct loss of follicles and earlier menopause.
- Alcohol excess: linked to hormonal disruption.
- Pesticides/heavy metals: shown to impair ovarian function.
- Occupational chemical exposure: risk varies by agent and dose.
- Poor diet/obesity: inflammation and metabolic stress affect follicles.
- Medical treatments (chemotherapy/radiation): high-risk for permanent damage.
Diagnosis Process
Diagnosis of diminished ovarian reserve requires a focused assessment of ovarian function using blood tests and ultrasound imaging. Accurate evaluation guides treatment choices and timing and helps set realistic expectations. The process integrates menstrual history, cycle-timed hormone measures, and antral follicle counts and should be tailored to age, prior surgeries, and individual medical history.
Blood Tests
Basic blood work consists of AMH, FSH, and estradiol. AMH indicates the number of small developing follicles. It’s highest in the mid-twenties and decreases with age. A low AMH, often labeled as less than 1.0 ng/mL, is associated with diminished ovarian response to stimulation and decreased IVF pregnancy rates.
FSH is measured on cycle day 2 or 3. A mildly elevated FSH, above roughly 12 mIU/mL, is worrisome for diminished reserve. The higher the values, the more concern. Estradiol is commonly drawn on those same days to ensure early-cycle estradiol isn’t artificially suppressing FSH and to assist in staging the cycle.
| Test | Normal range (cycle day 2–3) | Clinical significance |
|---|---|---|
| AMH | Age-specific: less than 1.0 ng/mL equals low | low AMH equals lower ovarian reserve, lower IVF success |
| FSH | ~3–10 mIU/mL normal, >12 mIU/mL mildly high | Elevated FSH indicates diminished ovarian reserve |
| Estradiol | 20–80 pg/mL normal early-cycle | High early estradiol can hide elevated FSH. |
Interpretation has to include lab technique and units. All AMH assays are different and units might be ng/mL or pmol/L.
Ultrasound Scans
Transvaginal ultrasound is the primary imaging study to count antral follicles. Antral follicle count (AFC) is typically performed in the early follicular phase. A normal AFC is about 8 to 11 follicles per ovary. Counts under that range, particularly fewer than 4 follicles per ovary in women over 40, point to decreased reserve.
Ovarian volume and the pattern of follicles add context. Small volume ovaries with few visible antral follicles reinforce the diagnosis. Ultrasound aids in watching response during controlled ovarian stimulation. A series of scans monitor follicle growth and quantity, guiding medication dose tweaks and scheduling of egg retrieval.
Previous oophorectomy or lesions can alter ultrasound appearance and account for diminished counts.
Interpreting Results
Clinicians integrate hormone tests and AFC rather than using a single value. Abnormal results forecast decreased response to stimulation and could impact the course of care. Options are modified stimulation regimens, earlier referral to IVF, or donor oocytes.
There are cutoff values for AMH and AFC that stratify patients into likely good, poor, or intermediate responders. Findings are evaluated considering age, previous fertility history, and potential factors such as surgery or endometriomas. Discussing what the numbers say about prognosis and next steps is key to personalized care.
Treatment Pathways
Treatment pathways for diminished ovarian reserve extend across medical, lifestyle, and assisted reproductive options. The path you’ll take depends on your age, measured ovarian reserve, overall health, previous response to stimulation, and personal goals. Here are the primary paths with actionable information, what to anticipate, and cases to help direct the decision making.
Own Eggs
With your own eggs, it typically translates to higher doses of fertility drugs and custom-designed stimulation regimens. Clinics may utilize GnRH agonists or antagonists, and higher gonadotropin dosing to recruit more follicles. Protocols differ and are selected based on previous cycle data and baseline hormone levels.
Success rates depend on egg quality and ovarian response. A 35-year-old with low reserve is very different from a 42-year-old. IVF with own eggs is still an option, but with diminished reserve, live birth rates are typically lower. Recording previous stimulation, medication variety, overall dose, follicle development, and eggs retrieved assists in optimizing subsequent cycles and preventing narcissistic, repeated head-banging.
Others incorporate supplements such as antioxidants or omega-3s and advise weight loss or smoking cessation to assist egg health.
Donor Eggs
Donor eggs are a sure bet when ovarian reserve or egg quality caps your yields. Donor cycles tend to have elevated pregnancy and live birth rates given donors are usually very young and fertility tested for egg quality. This involves donor selection, medical and psychosocial screening, matching, and synchronizing the recipient’s endometrium with the donor’s stimulation or frozen embryo schedule.
Donor eggs circumvent low egg count and poor quality, so results are more reflective of donor age than recipient age. For instance, a recipient in her 40s with fresh donor eggs can have live birth rates equivalent to the donor’s age group, typically far higher than what she could have achieved with her own eggs.
Embryo Adoption
Embryo adoption is taking frozen embryos donated by other couples and providing pregnancy without donor eggs or own eggs. Patients receive uterine preparation and embryo transfer as in frozen embryo transfer. Legal and ethical considerations involve consent forms, donor anonymity or contact preferences, and procedures for future contact.
Laws vary by country, therefore legal advice is frequently recommended. Advantages are cheaper than fresh donor cycles and known embryo quality. Disadvantages are lack of control over the source of embryos and varying medical histories on donors.
Child-Free Living
Declining additional treatments is a potential path. Counseling and peers help process grief and plan life goals. This option can be in sync with personal, career, or financial priorities and can seem empowering.
Other roads to satisfaction are possible, such as through mentoring, creative work, travel, or reproductive health advocacy.
Beyond The Clinic
DOR is more than a clinical diagnosis. Lifestyle, nutrition, and emotional health influence how a person experiences fertility and responds to treatment. These non-medical factors can bolster ovarian function, complement medical care, and sometimes improve your odds with timed intercourse or IUI, especially for younger folks with mild DOR.
Nutrition
A diet full of antioxidants can help support egg quality by reducing oxidative stress. Add bright vegetables, berries, nuts, and legumes on a regular basis. Minimize processed foods, added sugars, and trans fats that increase inflammation and can damage reproductive tissues.
Alcohol and high caffeine intake tie to worse ovarian results in certain research. Reducing intake can assist. Keep your body weight at a healthy level. Being underweight or obese can interfere with menstruation and ovulation.
Shift working women take note. Irregular shifts can seriously disrupt your hormonal rhythms. Try to be consistent when possible with your sleep!
Fertility-friendly foods to add: fatty fish (low in mercury) for omega-3, leafy greens for folate and iron, eggs for choline, and citrus for vitamin C. Vitamin D shows up in the research as supportive for ovarian function. Getting levels checked and correcting deficiency makes a difference.
Supplements
Folic acid and prenatal vitamins give you that baseline nutrient cover needed for egg and embryo health. Others such as CoQ10 and DHEA have some studies demonstrating improvement in ovarian response and embryo quality, but evidence is mixed. Timing, dose, and candidate selection are important.
Take supplements as part of a coordinated plan with your clinician. Random use minimizes advantage. Below is a straightforward table of popular supplements and their possible impacts.
- Folic acid and prenatal vitamins support neural development and general egg health.
- Vitamin D: may support ovarian function if deficient.
- CoQ10 may improve mitochondrial function in eggs, but some tests indicate improved reaction.
- DHEA is proposed to boost androgen levels and ovarian response in select cases.
- Omega-3: supports blood flow and lowers inflammation.
Mindset
Stress reduction can help fertility as well. Chronic stress can disrupt your hormone balance and your menstrual cycle. Mindfulness, meditation, or breathing exercises can help lower stress and improve coping.
Beyond The Clinic Counseling offers room to work through grief, frustration, and changing expectations, which can alleviate some of the emotional load during treatment.
Yoga and light exercise can both relieve stress and support sleep. Heavy exercise that causes energy deficit may injure ovulation. Control expectations. Work with your care team to establish realistic goals and plan emotional support as well as medical measures.
Support
Join support groups for shared experience, practical tips, and coping strategies. Peer groups don’t feel so isolating. When helpful, include partners and family in appointments and planning. Shared understanding makes decisions and stress easier.
Make a resource list of local and international organizations, counselors, and online communities. Clinical therapy tackles worry, relationship tension, and bereavement and can enhance resiliency through intervention.
The Emotional Reality
DOR delivers medical truths and an accompanying emotional reality that permeates life, love, and decision-making. The emotional truth is that individuals confront a cocktail of mourning, rage, and anxiety when fertility timelines are adjusted. That emotional weight frequently comes hand-in-hand with pragmatic worries about treatment expenses, job prospects, and parental aspirations. It can alter the way an individual rests, dines, or toils.
Understand the emotional reality of diminished ovarian reserve and infertility. Grief is universal, not just for lost pregnancies but for lost hope and lost time. Studies document infertile patients experiencing anxiety, depression, and diminished quality of life. Patients with adverse IVF outcomes exhibit greater state anxiety post-treatment. Such anxiety can linger and taint decisions about ongoing treatment.
In some cases, conditions linked to ovarian function, like Premature Ovarian Insufficiency, come with broader life stress. This includes trouble at work, strained family ties, and sleep problems that feed into emotional distress. Talk about the reality: grief, frustration, and loss of control. Frustration and loss of control are common emotions.
Women with POI are more susceptible to depression, and some of them are depressed up to five years prior to diagnosis, suggesting long-term mental health issues. Functional Hypothalamic Amenorrhea patients present with higher depression and anxiety test scores than healthy controls. High anxiety during IVF links to worse outcomes, including lower clinical pregnancy and fertilization rates.
Psychological stress can even accelerate the decline in ovarian markers like Anti-Müllerian Hormone in those with low positive affect, bringing emotions and biology full circle. To highlight the power of communication with your partners and loved ones, some frank, realistic discussion with a partner or trusted family relieves the isolation. Share practical needs, such as when to attend appointments, how to split research or costs, and when to seek a break from fertility talk.
Little compromises, like who takes messaging clinics and who goes to what visit, reduce stress. If talks get fiery, a neutral listener like a counselor can help draw lines in the sand and keep conversations rooted in common objectives and love. Push for community and professional support. Peer groups and online communities provide solidarity and practical advice.
Expert guidance is key. Cognitive Behavioral Therapy helps reduce stress scores in infertile patients and teaches tools to shift unhelpful thoughts, improve sleep, and enhance coping. Consider early screening for mood disorders, particularly if you have POI or long-term menstrual problems. Seek out therapists who work with reproductive care if possible to connect the emotional work with the medical actions.
Conclusion
Diminished ovarian reserve means a different path forward. It doesn’t erase options. Tests like AMH and antral follicle count provide concrete information. Fertility clinics use that information to establish a plan. That plan might involve timed cycles, IVF with customized stimulation, egg freezing, or donor eggs. Lifestyle moves such as regular sleep, an unprocessed diet, and dropping heavy smoking back up overall health and can aid fertility attempts. Emotional care remains essential. Peer groups, a few sessions of therapy, or a coach can relieve stress and help stabilize focus.
If you’d like a next step, book a consult with a reproductive specialist and bring along your test results. That meeting transforms data into a plan of action.
Frequently Asked Questions
What is diminished ovarian reserve (DOR)?
DOR means that your ovaries contain fewer eggs or eggs of reduced quality in comparison to the norm for your age. It reduces natural fertility and could impact responses to treatment.
How is diminished ovarian reserve diagnosed?
Clinicians evaluate diminished ovarian reserve with blood tests (AMH, FSH, estradiol) and ultrasound (antral follicle count). Tests are fast and inform fertility planning and treatments.
Does DOR mean I cannot get pregnant?
Not necessarily. Most DOR patients will conceive naturally or with treatment. It all depends on age, egg quality, and your chosen fertility strategy.
What treatment options are available for DOR?
Options range from timed intercourse to ovarian stimulation with IVF, donor eggs, or preservation. A specialist in fertility will advise the optimal route for you.
Can lifestyle changes improve ovarian reserve?
Lifestyle factors (healthy weight, stop smoking, reduce alcohol, balanced diet) support fertility but don’t increase egg number much. They can enhance general reproductive wellness.
How does age affect DOR and fertility outcomes?
Age is a very important factor in egg quality and IVF success. Younger DOR patients tend to do better than older patients who have similar ovarian reserve tests.
What emotional support is available for people with DOR?
Counseling, support groups and fertility coaches assist with stress and decisions. Mental health care is shown to enhance coping and treatment compliance.
