Posted November 07, 2025 in Fertility Blog & Information
17 minute read
Key Takeaways
- PRP employs a concentrated sample of the patient’s own platelets to deliver growth factors that can stimulate endometrial cell growth and repair. This provides a biologically plausible option for thin uterine lining.
- Local evidence, such as reports from Houston clinics, indicates that there are measurable increases in endometrial thickness and some patients have better implantation rates. These results are frequently shared with thorough study methodology and patient information.
- The procedure is minimally invasive, conducted in the office with sterile technique and encompasses defined preparation, ultrasound-guided delivery, and follow-up to gauge lining response.
- Best candidates are patients with recurrent implantation failure associated with thin lining or endometrial scarring. Those with active infection, hematologic disorders, or malignancy must be ruled out after adequate examination.
- Practical considerations include variable costs frequently paid out-of-pocket and confirming insurance coverage or financing options before treatment.
- Next steps: Consult a fertility specialist to review local outcome data, verify candidate suitability with testing, discuss personalized protocol and expenses, and schedule follow-up imaging to monitor endometrial response.
PRP for thin lining Houston
Dosing Houston
PRP for thin lining evidence suggests PRP can help endometrial growth in some studies. Clinical reports and small trials document thicker lining and higher implantation rates after PRP, but sample sizes vary.
Most studies utilize intrauterine PRP prior to embryo transfer and report lining in millimeters. Patient factors and protocol variations impact the results.
The main body summarizes and evaluates the Houston studies, the methods, and practical considerations for clinics.
Understanding PRP
Platelet-rich plasma (PRP) is a concentration of platelets from the patient’s own blood. It is rich in growth factors and cytokines that can stimulate tissue repair and cell proliferation. PRP has attracted interest in areas like orthopedics, dermatology, and reproductive medicine, where it can promote local healing without adding any foreign substance.
In fertility medicine, doctors consider PRP when the endometrial lining is thin and unresponsive to traditional hormonal or adjunctive interventions.
The Science
PRP is rich in growth factors, including platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-β), vascular endothelial growth factor (VEGF), and epidermal growth factor (EGF) that stimulate cell proliferation and tissue regeneration. These bind to receptors on endometrial stromal and epithelial cells, triggering pathways that promote cell division and matrix production.
Transcriptomic profiling of human endometrial stromal cells treated with autologous PRP reveals changes in gene expression associated with epithelial regeneration and cell signaling, providing a molecular-level understanding of its mechanism of action.
Biologic mechanisms likely include increased angiogenesis, stromal cell proliferation, and local immune modulation. Platelet-derived cytokines aid in inflammation and healing, decreasing a hostile microenvironment that can compromise implantation.
In other words, the hypothesis is that delivering a concentrated dose of endogenous growth factors directly into the uterus has the potential to reestablish a receptive lining and support embryo implantation in situations where it previously could not be accomplished.
The Process
- Draw around 20 mL of venous blood from the patient’s upper arm into a citrate anticoagulant-containing syringe, such as acidic citrate A (ACDA), to preserve platelet function.
- Centrifuge the blood with a standard two-step protocol. A typical setting is 400 times the force of gravity for 10 minutes at 21 to 24 degrees Celsius to prevent early platelet activation.
- Isolate the platelet-rich layer, sometimes with a second spin to concentrate platelets and generate the final PRP volume.
- Ready the uterine cavity under sterile conditions, clinically, and inject PRP through a catheter. The procedure is non-invasive.
- Follow up with the patient post-procedure and retreat per clinic protocol as needed.
Sterile technique is required throughout to avoid infection and maintain efficacy. Adequate centrifuging and anticoagulant use create the high platelet concentration and active growth factor profile.
The Goal
The primary aim is to increase endometrial thickness to improve implantation rates. Other goals involve promoting uterine receptivity and early embryo development.
- Promote measurable endometrial growth within a treatment cycle.
- Improve blood flow and microvascular density in the lining.
- Reduce local inflammation and normalize cytokine balance.
- Offer an option after failed conventional therapies.
In brief, while PRP appears to promote endometrial growth and improve pregnancy outcomes in many studies, results are still inconsistent and more research is needed to optimize protocols and determine long-term effects.
Houston Evidence
Houston, a Hub for Applied Fertility Research and PRP for Thin Lining. Several clinics and academic groups in the region have gathered patient information, conducted prospective cohorts, and published results through December 2022, generating 36 original articles that guide local practice and enable comparison to global data. This local evidence helps clinicians tailor protocols to the needs of the region’s diverse patient population and supports collaborative studies with research institutions.
1. Local Studies
A few Houston trials focused on women with refractory endometrium or repeated implantation failure (RIF). One study involved 20 women with a mean age of 33.4 ± 5.7 years undergoing frozen embryo transfer (FET) after previous RIF. Houston Evidence Molina et al conducted a prospective study of 19 patients aged 33 to 45 with refractory lining, reporting measurable changes post-PRP.
Across studies, injection volumes into the endometrium were commonly low; 11 studies were up to 1 ml. For uterine cavity injections, the initial blood draw was 8 to 20 ml and for ovarian protocols aspirated volumes were from 8 to 50 ml. Study durations differed but generally spanned the treatment cycle plus early pregnancy follow-up. Sample sizes were modest, with most in the tens rather than hundreds, precluding wide generalizability but providing helpful clinical signals.
Wherever possible, Houston results were contrasted with national or international series and on the whole demonstrated comparable trends of lining enhancement and elevated pregnancy metrics.
2. Patient Outcomes
After PRP, numerous Houston patients experienced statistically significant ultrasound increases in endometrial thickness either that same cycle or the next. Clinics experienced fewer cycle cancellations due to thin lining following PRP protocols. Implantation and pregnancy rates were higher in treated groups compared to controls in multiple cohorts.
Patient-reported experience generally cited low pain at injection and great satisfaction when lining improved. Some patients indicated less stress associated with fewer cancelled cycles. Not all reports recorded standardized symptom scales, so subjective reports differ in detail.
3. Success Rates
In pooled local results, the PRP group showed higher pregnancy metrics. Chemical pregnancy was 53.06% versus 27.08% in controls, and clinical pregnancy was 44.89% versus 16.66%. These numbers represent particular groups through December 2022 and are to be considered in conjunction with small samples.
Some studies reported subgroup breakdowns by age or diagnosis, with younger patients and those without severe uterine pathology tending to fare better. Visual comparisons in clinic reports used tables to display pre and post rates and subgroup comparisons.
4. Research Methods
Houston teams utilized collected patient data, taking histories, details of cycles and responses, in a more structured manner. A few studies had endometrial biopsy for histology and immunochemical assays to follow changes in cellular markers after PRP.
Statistical methods varied from paired t-test to chi-square and regression models to evaluate efficacy and safety. A glaring omission was the inconsistent report of the day of the menstrual cycle for PRP administration in ovarian protocols, which impedes accurate protocol standardization.
The Procedure
The procedure focuses on intrauterine infusion of platelet-rich plasma (PRP) to thicken the endometrium in thin-lined patients. It is minimally invasive and divided into three phases: preparation, administration, and aftercare. Timing and individual protocol modifications vary, and therapies are typically administered in a hormone replacement or natural cycle under ultrasound direction.
Preparation
Patients have standard blood work to screen for infection, anemia, and coagulation problems prior to PRP harvest. For the infusion, 17.5 mL of peripheral venous blood is withdrawn into a syringe with 2.5 mL ACD-A anticoagulant, a total volume of 20 mL.
Fasting is generally not mandatory at most clinics; however, patients are usually requested to hydrate well in order to facilitate venous access and decrease the likelihood of lightheadedness. Upon collection, it is immediately centrifuged at 1,200 rpm for 12 minutes to separate red blood cells and concentrate platelets.
Other processing steps involve careful layering, transfer of the PRP fraction, and volume and appearance checks. Clinicians verify that syringes, needles, and the centrifuge are sterilized and validated. They’re customized. For instance, patients with previous bad response may receive tweaks in PRP volume or timing, and patients on blood thinners need individualized scheduling.
Administration
PRP is applied through intrauterine infusion, generally under ultrasound or hysteroscopic guidance to guarantee precise delivery. A 35 to 40 mL aliquot of PRP is instilled via an endoscopic needle injection during the proliferative phase, typically day 6 to 9 of the cycle before transfer.
The initial infusion is typically given the same day as the blood draw, approximately cycle day 9 or 10 at many centers. The procedure itself typically only requires 15 to 30 minutes from catheter placement to completion, and patients experience mild cramping or pressure but otherwise tolerate it well.
Local anesthesia or cervical block can be provided for ease in specific cases. With real-time imaging, they make certain the PRP enters the uterine cavity and not accidentally somewhere else, adjusting angle and depth as they observe the infusion spread.
Aftercare
Patients relax for a short period after the procedure, then head home from the clinic and can typically resume light activities that same day.
- Avoid heavy lifting or vigorous exercise for 24–48 hours.
- Use mild analgesics if needed; avoid NSAIDs if instructed.
- Refrain from intercourse for 48 hours or as per clinic recommendation.
- Continue prescribed hormone replacement: estradiol valerate and micronized progesterone as directed.
Watch out for fever, heavy bleeding, severe pain, or unusual discharge and notify immediately. Endometrial thickness is rechecked 3 to 5 days after infusion, and if it remains less than 7 mm, a second PRP infusion may be performed.
Few studies report on the actual percentage of patients achieving 7 mm or more after PRP, with approximately 64.7% reported in one study, but it varies considerably by protocol and patient factors.
Patient Suitability
Patient suitability identifies patients who can realistically anticipate advantage from intrauterine PRP for thin endometrium. A brief clinical overview helps frame specific eligibility. PRP is considered when standard hormonal and mechanical measures fail to achieve an adequate endometrial thickness (EMT), particularly for women preparing for frozen embryo transfer (FET).
Thoughtful patient selection finds those most likely to benefit and screens out conditions that would alter care or cause PRP to be unsuitable.
Ideal Candidates
- Repeated IVF or FET failures occur in the context of persistently thin lining despite conventional treatments.
- Previous cancelled cycles due to endometrium less than 7 mm even with estrogen therapy or adjuvant measures.
- Thin endometrium recorded on ultrasound, such as EMT less than 6 mm in previous cancelled cycles.
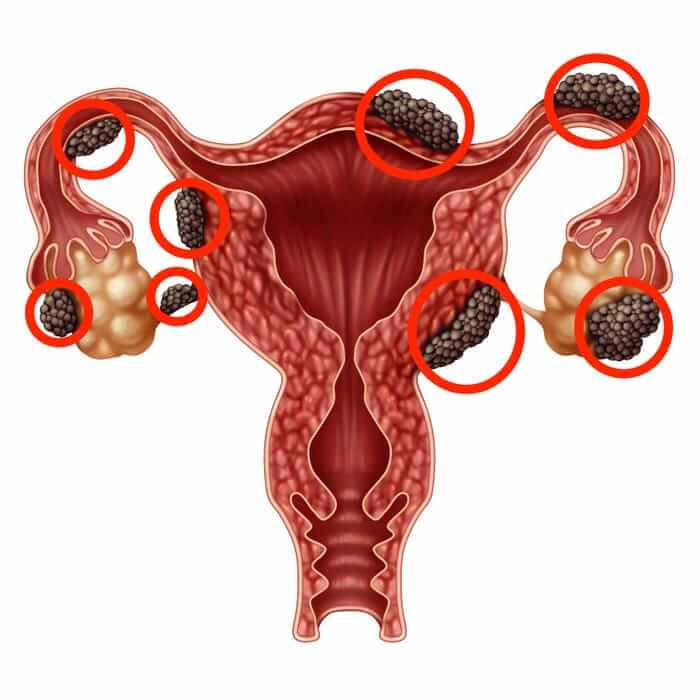
- Women with Asherman’s syndrome or known intrauterine adhesions that result in endometrial scarring.
- Patients looking for a low-risk autologous adjunct to optimize lining prior to embryo transfer.
- Absence of active pelvic infection or known uterine malignancy.
- Reasonable systemic health without severe uncontrolled medical disease.
EMT data suggest a few patients with EMT less than 7 mm still get pregnant after PRP. For example, a cohort had 26 live births, 18 of whom had EMT greater than or equal to 7 mm and 8 with EMT less than 7 mm.
Single-arm studies of patients with prior EMT less than 6 mm have demonstrated encouraging responses, indicating PRP may widen the realm of possibility for those previously considered poor responders.
Contraindications
Absolute contraindications are known platelet dysfunction or blood disorders that significantly impair clotting or platelet function.
PRP should not be used if there are signs of active pelvic or systemic infection. Putting intrauterine matter could exacerbate infection and affect implantation.
Severe systemic illnesses, for instance uncontrolled autoimmune disease or decompensated cardiac, hepatic or renal failure, are a caution. These conditions can affect healing and add procedural risk.
Allergy to any component used in PRP processing or local anesthetics applied during the procedure is also a contraindication.
Patients with uterine or endometrial malignancy should not receive PRP as growth factors can theoretically stimulate neoplastic cells. In very thin lining less than 6 mm, a few cycles have been cancelled even after PRP, so not all thin lining will respond.
Three reported cycles were discontinued for refractory EMT less than 6 mm despite perfusion. Clinical decisions must balance the likelihood of benefit against these risks, and patients need transparent counseling on variable rates of success and the potential for multiple cycles.
Beyond The Data
PRP for thin endometrium poses questions that statistics can’t answer. Clinical measures follow thickness, vascular indices and pregnancy rates, but they omit the patient experience, nuances of clinical decisions and how therapies transform everyday life. Its subheadings, below, explore those non-numeric elements, weaving in up-to-date research while keeping lived experience and real-world consequences at the forefront.
The Human Element
Trust between patients and providers influences PRP adoption and the interpretation of results. Patients choosing autologous PRP contemplate inconclusive data versus past heartbreaks. Transparent articulation of risks, benefits and alternatives counts.
Personal attention—scheduling PRP injections, dose selections, synchronization with hormone cycles—impacts both efficacy and patient trust. Emotional investment runs deep in fertility care, and clinicians who listen, explain uncertainty, and set realistic expectations can reduce confusion and help patients stay engaged.
Resilience shows in narratives: people who pursue PRP after repeated thin‑lining diagnoses often describe determination rather than blind hope. Those stories inform clinicians about tolerable side effects and acceptable protocols. These anecdotal accounts direct care decisions in the absence of large, definitive trials.
Emotional Impact
Just the act of having a new option like PRP can provide quantifiable relief before results even manifest. For a lot of patients, the hope of a treatment to help endometrial development shortens acute anxiety associated with every cycle.
Although anecdotal, following positive results some experience reduced baseline stress and increased sense of control, which can promote better treatment adherence. A string of failures inflicts a heavy emotional price—disappointment, guilt, exhaustion—and PRP is occasionally painted as a restoring remedy that revives hope.
Counseling and peer support augment medical care. When clinics incorporate psychological help, patients say they cope better and make decisions more clearly. These psychosocial benefits do not replace hard data, but they are important for quality of life and for how patients judge a treatment’s value.
Future Hope
Research into PRP’s mechanisms, growth factors, cytokine modulation, and effects on receptivity continues, and protocol refinement is probable. As more controlled trials get published, access might broaden, shifting PRP from experimental to approved adjunct in some cases.
Combining PRP with other regenerative approaches, such as stem-cell based therapies or novel hormonal timing, is in early study and may enhance results for refractory endometrium. Evidence is mixed; some studies show improved thickness and lower early loss with PRP, while others find no vascular change versus controls.
A study cited a 2.4-fold higher early loss with conservative therapy compared with PRP-inclusive regimens. Ongoing trials will help elucidate which patient populations receive the most benefit and the optimal dosing and timing. Innovation in reproductive medicine tends to proceed in these incremental steps, informed by a mix of controlled data and patient experience.
Financial Considerations
PRP for thin endometrium has direct and indirect costs that influence access and approach. Financial considerations cover procedure fees, associated clinic costs, the potential for repeat treatments, and how it compares to other fertility alternatives. Here’s a lens on those factors to assist you in making practical decisions.
Treatment Costs
Typical PRP procedure fees in Houston generally range from 500 to 2,000 (USD) per treatment, depending on clinic reputation, kit used, and whether an anesthetic or imaging is needed. Some clinics charge around 500 to 800 for a basic outpatient injection, while specialty centers or academic-affiliated providers may charge 1,200 to 2,000.
Additional fees often include an initial consultation of 50 to 300, blood draw and lab processing of 100 to 400, and any ultrasound guidance during the procedure of 75 to 300. Follow-up visits for assessment and repeat ultrasound can add 50 to 200 per visit. Multiple sessions are common; some patients have two to three treatments spaced across a cycle, which multiplies the base cost and can push total spending into the several thousands.
A simple table shows typical costs by therapy type:
| Service | Typical cost range (USD) |
|---|---|
| PRP injection (single) | 500–2,000 |
| Initial consult | 50–300 |
| Lab processing/blood draw | 100–400 |
| Ultrasound guidance | 75–300 |
| Hormone therapy adjuncts | 100–600 |
| Endometrial scratch / other local therapies | 200–1,000 |
| IVF cycle (fresh) | 8,000–15,000 |
| IVF with donor eggs | 15,000–30,000+ |
Clinics occasionally provide package deals that combine consultation, two PRP sessions, and follow-ups for a set fee or discounts for upfront payment. There may be some promotional pricing depending on the month or for patients being referred through networks. Inquire at clinics about bundled pricing, sliding scales, or low-fee trials.
Insurance Landscape
Most insurance plans will not cover PRP for thin lining because it is considered experimental or not standard of care. Patients should anticipate paying out of pocket. Out-of-pocket expectations are the procedure cost plus clinic fees.
A couple of pilot programs or research studies in Houston may subsidize some expense under study protocols, but these are few and have eligibility criteria. Check benefits with your insurers prior to treatment.
Look into financing options like medical credit cards, clinic payment plans, or fertility loans that amortize payments. Save receipts and paperwork, as occasionally insurers will re-review allied coverage if linked to an approved infertility diagnosis.
The price of PRP dictates treatment selection, particularly where repeated treatments are probable. Research indicates PRP can lower the requirement for subsequent IVF cycles; however, overall long-term financial viability is still being studied.
Conclusion
PRP provides a low-risk possibility for thin lining individuals. Houston PRP for thin lining evidence shows a modest increase in thickness and increased odds of implantation in some patients. Clinic reports state quicker recovery and minimal side effects. Ideal candidates have mild thinning, excellent egg quality, and no significant uterine pathologies. Expect one to three cycles and clear steps: blood draw, spin, and ultrasound-guided injection. Prices differ, and it is not a sure thing.
For an actionable immediate step, review your ultrasound and hormone reports. Talk to your physician for local data, precise protocol, and success rates in cases similar to yours. Book a consult to weigh PRP against alternatives like hormonal therapy or surgical repair. Get a second opinion if results are ambiguous.
Frequently Asked Questions
What is PRP and how can it help a thin uterine lining?
PRP (platelet-rich plasma) uses concentrated growth factors from your blood. Injected into the uterus, it might stimulate repair and enhance endometrial thickness, helping implantation in certain patients.
What evidence supports PRP for thin lining in Houston clinics?
Houston clinics tout thin lining case series and small studies of improved lining and pregnancy. There are still only a few high-quality randomized trials. Request published data and outcome rates from your clinic.
Who is a good candidate for PRP treatment?
Candidates have persistently thin endometrium despite conventional treatment. You cannot have an active infection, and you need to be seen by a fertility specialist to ensure it is a good fit.
What does the PRP procedure involve and how long does it take?
Blood draw and centrifuge to isolate PRP, then ultrasound guided intrauterine infusion. It lasts approximately 30 to 60 minutes and requires little recovery.
Are there risks or side effects of intrauterine PRP?
Side effects are uncommon and usually mild, including cramping, spotting, or infection risk. Because it’s your own blood, it lowers allergic risk. Talk about your personal risks with your provider.
How many PRP treatments are typically needed and when are results seen?
Protocols differ. Most clinics do one to three infusions per cycle. Certain patients observe lining enhancement in a matter of days to a couple of weeks, but results vary.
How much does PRP for thin lining cost in Houston and is it covered by insurance?
Prices differ drastically between clinics and are usually out of pocket. Insurance coverage is rare. Get a detailed fee estimate and inquire about package pricing or financing.
