Posted July 31, 2025 in Fertility Blog & Information
15 minute read
Key Takeaways
- Digital ovulation monitors are more accurate by identifying critical hormones such as LH and estrogen, which allows them to pinpoint a user’s most fertile days.
- Clinical research backs up digital monitor reliability, with many users reporting enhanced insight and monitoring of their fertility trends.
- Used properly — same time, right sample — it can produce accurate results and effectively inform your fertility awareness.
- Things like irregular cycles, health conditions and device quality don’t always muck with monitor accuracy, so users should be aware of these factors and consult a medical professional if necessary.
- Finding a balance between data accuracy and emotional well-being. Open conversation and encouragement throughout the fertility journey can keep stress in check.
- With continuous innovations in sensor technology, AI, and wearables, digital ovulation monitors will only become more accurate and personalized in the years to come.
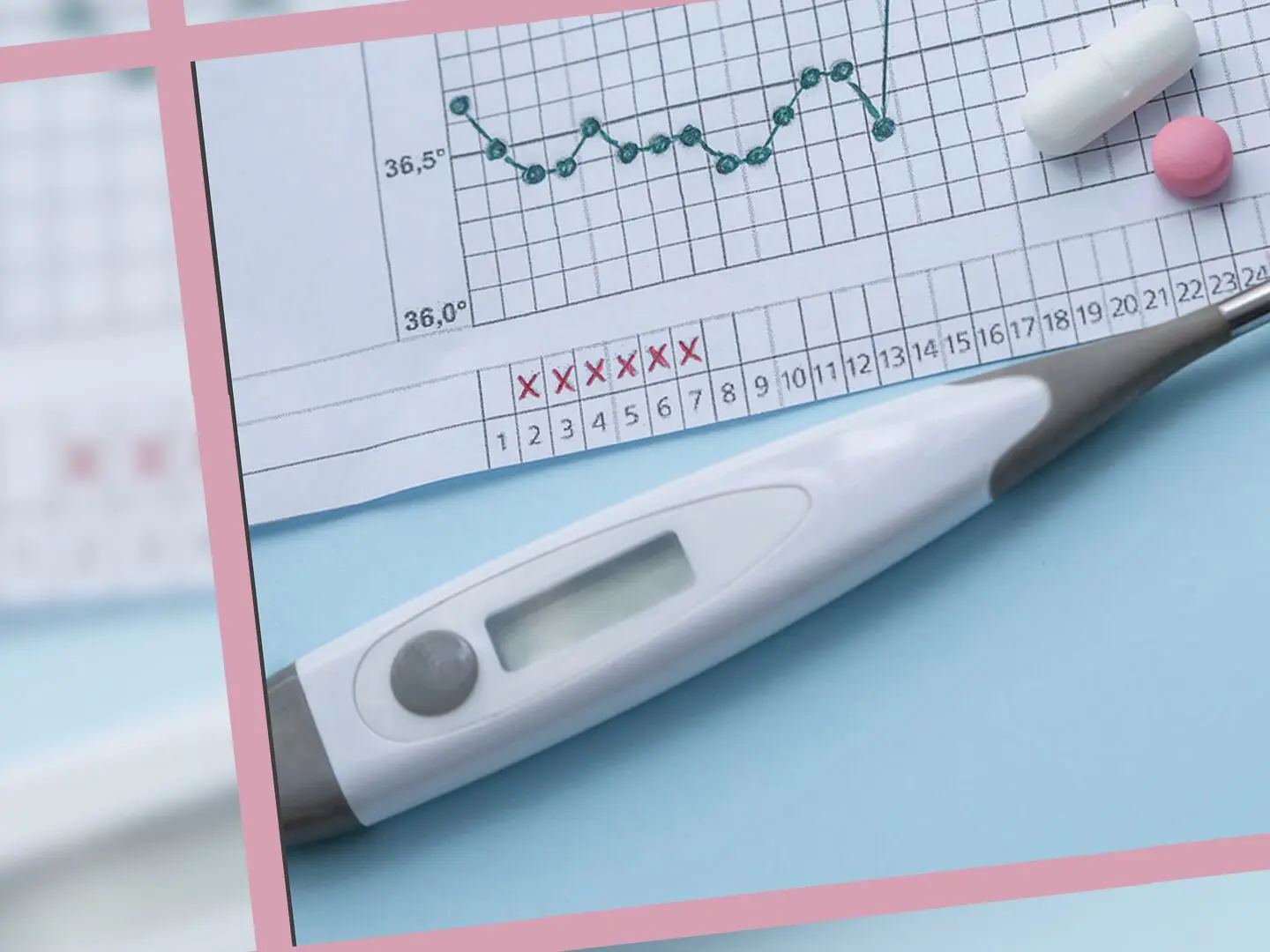
Digital ovulation monitor accuracy refers to how accurately these smartphones can identify your fertile window by monitoring hormonal fluctuations in urine or saliva. The majority of digital ovulation monitors exhibit an accuracy rate exceeding 97% in identifying the LH surge, which typically indicates the onset of ovulation. With clear display screens and simple controls, they’re easy to use for daily home use. Some follow additional hormones to provide a more comprehensive picture of the cycle, while others connect to tracking and reminder apps. Results may vary with use, timing or user health, so eating your instructions is essential. To understand what impacts digital ovulation monitor accuracy, the main section will detail how these devices operate, what users can anticipate, and advice for optimal outcomes.
Monitor Precision
Digital ovulation monitors target your most fertile days by measuring hormones associated with ovulation. Instead of simple test strips, these devices provide a closer view of hormone fluctuations and utilize algorithms to assist users in interpreting patterns. Their accuracy relies on trusted hormone readings, clinically validated outcomes, and the adaptability of their technology to individual users and cycles.
1. Hormone Detection
Digital ovulation monitors track pivotal hormones such as luteinizing hormone (LH) and estrogen, while a select few monitor the progesterone metabolite PdG. These hormone fluctuations define the fertile window and indicate when ovulation is approaching.
Precision counts. Their 2017 review determined that urinary LH, estrogen-estradiol (E-1-3-G), and progesterone (PdG) were the best predictors for both upcoming ovulation and confirming it has occurred. With up to 99% accuracy in select monitors, these measurements help users have trust in their results. Urinary hormone testing, however, extends beyond calendar tracking by providing real-time data, allowing individuals to identify when their fertile window begins. This can display as four or more fertile days, though users will occasionally notice longer windows — particularly if cycles are irregular or impacted by health issues like PCOS.
2. Clinical Data
Science confirms the edge from digital monitors. In a 2007 study, women using a monitor were nearly twice as likely to conceive within two cycles as those who didn’t use one.
This increase in pregnancy rates connects to improved timing and knowledge of the fertile window. Clinical trials demonstrate high accuracy for digital monitors, but variables such as age or medical conditions can impact performance. User reports from research participants regularly indicate increased confidence and reduced stress with monitors versus just ‘throwing darts’ for ovulation days.
3. Method Comparison
While digital monitors utilize sensors and transparent screens, traditional line tests still depend on color variation. The gold standard continues to be the LH test strip. Digital alternatives bring added precision, less ambiguity and frequently monitor multiple hormones.
These are great for those with irregular cycles since they adapt to hormonal patterns. There are even digital kits that can display more than nine high-fertility days — which doesn’t necessarily equate to ovulation. Monitoring cervical fluid, as demonstrated in a 2013 study — makes those pregnancy rates better — when paired with hormone tracking.
4. Algorithm Role
Algorithms spot trends and adjust for each user.
Machine learning helps monitors get better over time.
With personalized data, your monitor can flag high fertility days with greater assurance.
Precision drops if cycles are very unpredictable.
Accuracy Influencers
There are many factors contributing to the accuracy of digital ovulation monitors. Both boilerplate habits and device features factor big. Outdoor conditions and illness modify the effectiveness these monitors. Most online influencers don’t talk about the limitations or dangers of these tests, and it’s important to look past social media hype.
User Factors
Manual reading is the trick. Even minor errors—such as using the wrong urine sample, testing at different times or missing days—alter results. A lot of users don’t realize that adhering to instructions is as important as the actually device.
Highly variable cycles month-to-month may make digital monitors unreliable. These gadgets thrive on routine. If cycles are erratic, predictions are apt to be wrong.
Testing daily, around the same time, aids monitors interpret hormone shifts more accurately. Testing or time change gaps can provide misleading results. Stress, overeating or under eating, and rapid diet changes can all cause hormone levels to fluctuate. These things can give confusing readings.
Device Factors
A not all digital ovulation monitors are created equal. Some employ superior sensors, more sensitive strips, or boast smarter software. Price doesn’t always equal better, but quality does.
Every device must be configured and tested. Bad calibration causes incorrect hormone readings. Test sticks designed for the incorrect brand or model may result in false readings.
Old batteries, dust, or simply not having been cleaned can impact its performance. Little things like this can make a pretty good monitor yield poor or inconsistent results.
Health Conditions
Health problems can complicate ovulation tracking. For instance, those with PCOS frequently have elevated hormone levels throughout the month, which can fool monitors.
Certain hormonal disorders, such as thyroid problems, can cause false peaks or missed fertile days. Certain other medications, like fertility or depression medicines, may alter hormone readings and confuse the device.
Physicians can assist identify if an underlying problem is transforming outcomes. It’s wise to consult a professional before trusting a digital monitor alone.
Best Practices
Ovulation
Frankly, these digital ovulation monitors can help track by detecting changes in hormones, typically the luteinizing hormone (LH) surge, which typically occurs 24–36 hours before ovulation. Their precision is contingent upon utilization, the user’s cycle consistency, and result interpretation. For best results, follow these guidelines:
- Test at the same time each day.
- Use first morning urine to obtain the most precise measurements.
- Follow instructions for urine collection closely to avoid contamination.
- Here are the best days to test – track your cycle length to find out.
- Keep a log of results and patterns.
- Think about using additional means (like basal body temp or cervical mucus) for more information.
- Be mindful of the pros and cons of each approach.
- Use disposable test sticks for hygiene.
- Seek medical advice if results seem unclear.
Consistent Timing
Testing at the same time each day is crucial for obtaining consistent, dependable hormone values. Hormone levels can shift rapidly so testing at varied times can provide conflicting or ambiguous results. The first urine of the morning is optimal since it is more concentrated and therefore more likely to display hormonal changes, such as the LH surge that indicates ovulation is impending. If you test later in the day or at other times, you might miss the surge, resulting in less accurate results.
Monitoring your cycle length allows you to choose the optimal days to commence testing. For irregular cyclers, you may have to test earlier and keep testing longer. Frequent tracking simplifies ovulation detection. Ovulation tests, timed well, can be proven to be very accurate (99%) in detecting the LH surge.
Correct Sampling
It counts to collect urine right. Wash your hands, grab a fresh cup if necessary, and direction on your test. Do not touch test stick tip or allow to touch surfaces. This avoids contamination and false positives. Hydrate but don’t guzzle immediately before testing, it can dilute your urine and make hormone levels tricky to interpret.
Always test with a new, disposable test stick. This keeps together results nice and neat and lowers potential for mistake.
Data Interpretation
- Compare the reading to the result guide.
- Contrast multiple days’ data to identify trends, not just individual readings.
- Record every outcome to assist identify patterns and forecast upcoming cycles.
- Leverage the monitor’s peak readings to schedule intercourse for maximum fertility.
Patterns in hormone levels over multiple cycles often give more insight than relying on a single result. Combine your digital readings with other signs, like cervical mucus or basal body temperature, for a fuller picture. Remember, basal body temperature alone is less accurate (only about 22.1%). Cervical mucus tracking is moderately accurate (48–76%), but may not work for everyone, especially those with infections. Transvaginal ultrasound is the gold standard but is less accessible and costs more.
Beyond The Data
Digital ovulation monitors are about more than just number-crunching. Their involvement in fertility monitoring is intimate, mixing information with lived feeling and everyday decisions. The path is seldom direct and every user’s story is influenced by a multitude of aspects.
Emotional Impact
Fertility tracking can be stressful, particularly when cycles shift or results don’t align with your expectations. Hormone shifts can contribute to mood swings and emotional volatility. Others feel strain in their relationships, particularly if tracking takes center stage in the household. Candid conversations with partners about emotions can relieve some stress and make both feel supported. Mindfulness, whether in the form of breathing exercises or brief walks, can help control stress on difficult days.
Accuracy vs. Utility
Digital monitors can be very exact, but real life is rarely perfect. One device may detect a fertile window reliably, but in daily use it can be less obvious if cycles are irregular. Some users seek precise, solutions-oriented answers, while others value small, quick-and-dirty utilities. Selecting a technique needs to correspond with your own needs–whether that’s deeper data or simply a general guide. Striking a balance between trusting the numbers and being user-friendly and providing peace of mind is often the recipe for success in the long run.
Holistic Journey
Taking a step back and looking at fertility as a journey, not just numbers, keeps users grounded. Lifestyle differences – such as improved sleep, reduced stress, and consistent exercise – can all contribute to reproductive health. Nutritious food—imagine well-rounded meals rich in greens and proteins—could back up hormonal equilibrium. A doctor or fertility specialist can provide guidance that complements each individual’s history, making it more manageable.
Inherent Limitations
Digital ovulation monitors assist some, yet they’re not without limitations. These devices may be less accurate in a variety of situations, such as irregular cycles, anovulation, or device errors. Knowing these boundaries is crucial for users seeking consistent output.
Irregular Cycles
- Monitor cycles for a minimum of a few months to identify patterns.
- Keep symptoms and physical observations, not just device metrics.
- Prefer a calendar app or paper diary for greater specificity.
- Be patient; cycle patterns often shift over time.
- Consider secondary ovulation signs, like changes in cervical mucus.
- Partner with a healthcare provider to review cycle data.
Folks with irregular cycles might experience inconsistent results. Devices frequently utilize hormone surges but if cycles aren’t consistent, these surges might not align with ovulation. Patience, my friends, tracking over months provides clarity. Care providers can assist in customizing approaches for those with persistent problems, providing guidance beyond what in-home devices are capable of.
Anovulation
Anovulation refers to the absence of ovulation. This can occur even if cycles appear regular. For a monitor, flat hormone readings with no obvious surge can indicate that you’re anovulatory. No ovulation, no fertile window, less useful tracking.
If patterns indicate anovulation, seek medical attention. If you continually miss surges or have inconclusive results, it’s time to see a healthcare professional. Knowing your own cycles is critical. Some girls have anovulatory cycles and this can throw a wrench in your plans.
Technical Errors
- Clean the monitor’s sensors and keep it dry.
- Double-check battery levels and replace batteries when needed.
- Reboot the phone if it locks up or spits weird answers.
- Contact customer support if problems keep happening.
Device glitches can throw off results. Occasionally, a quick reset or battery test resolves problems. Failing to update software or follow care tips can make readings less reliable. Keep it updated and read the manual for best results.
It helps to follow the instructions and keep the device clean. Even with careful maintenance, technical glitches may occur, so be sure to double-check strange readings prior to any major actions.
Future Innovations
Digital ovulation monitors are advancing rapidly, aided by emerging technologies. These shifts could assist individuals in monitoring fertility periods with greater accuracy, convenience, and simplicity. Future devices will probably test hormones at home, employ superior sensors, and integrate with wearables for a comprehensive view of reproductive well-being.
Sensor Technology
New sensors can pick up tiny hormone shifts in real time. Devices using these sensors might measure luteinizing hormone (LH) and estrogen in saliva, sweat, or urine, making the process less invasive. Better sensors could mean earlier warnings and fewer false readings for users. For example, skin patches or intravaginal biosensors are being studied to spot hormone changes every hour, not just once a day. This kind of tracking could help users see patterns they never noticed before.
With this progress, consumers could receive real-time feedback on their cycle, simplifying planning or preventing conception. Real-time data allows users to identify missed ovulation or irregular cycles immediately, enabling prompt consultation with a healthcare provider if necessary. Over time, sensors might connect with applications to provide users with a more seamless, transparent experience.
AI Integration
AI can sift through all that information and identify patterns that humans could overlook. Smart algorithms could examine hormone levels, temperature and even sleep to help make smarter predictions. With machine learning, the more you use the device, the better it knows your personal cycle.
Personalization will be crucial—AI could soon provide advice for individuals, not just the mean. For example, alerts could calibrate to someone’s previous cycles, stress or health fluctuations. More folks can be assured about their fertility awareness as the system adapts to what it learns.
AI might also assist users by interpreting what their data signifies — whether it’s indicating positive trends or potential red flags. With the data made readable, users remain engaged and can make wiser decisions.
Wearable Devices
Wearables are transforming fertility tracking. Wristbands and skin patches can now monitor HRV, temperature, and even respiration. These tools can monitor hormone changes all day, not just at select times.
For most wearables slot into natural rituals — wear and go. They can even link with ovulation monitors and health apps, providing a more comprehensive picture of cycles, sleep, and stress. This helps to visualize how everyday habits could impact fertility.
With more devices entering the market, users have more options to monitor and potentially better understand their health. Others now integrate HRV, temperature, and hormone levels for more accurate insights.
Conclusion
Digital ovulation monitors provide explicit information which many women find easy to use. Most demonstrate great performance, but ultimately, no device can interpret the human organism with absolute confidence. Others experience improved tracking with daily use, set times and taking notes. Some others prefer to blend tech with old-school methods such as charting or consulting a doctor. New upgrades continue to roll out, with apps and improved test strips, so the options just keep expanding. Everyone has a different objective, therefore requirements change. Looking to maximize your monitor? Make observations, listen to your body, and get in touch if you knock a snag. Post your own advice or questions for us and others on this same path.
Frequently Asked Questions
How accurate are digital ovulation monitors?
Digital ovulation monitors are usually more than 90% accurate in detecting hormone changes. Accuracy varies, based on proper use and brand.
What factors can affect the accuracy of a digital ovulation monitor?
Things like irregular cycles, medications and human error can influence results. Remember, always adhere to the directions the device provides and seek out your clinician if you’re uncertain.
Can digital ovulation monitors be used by everyone?
Digital ovulation monitors are most effective for women with regular cycles. Anyone with health conditions or irregular cycles may obtain less reliable readings.
How can I improve the accuracy of my digital ovulation monitor?
Take the monitor to the same time every day, heed all directions, and don’t down tons of liquids immediately before testing. Regularity is essential for accurate readings.
Are digital ovulation monitors better than manual methods?
Digital monitors can be more accurate than manual tracking, such as with calendar methods or basal body temperature. They give unequivocal, user-friendly results to most users.
What are the limitations of digital ovulation monitors?
They can’t promise pregnancy or diagnose fertility issues. Things like hormone imbalances can affect accuracy. For full fertility guidance, always consult a healthcare professional.
Will future technology improve digital ovulation monitor accuracy?
Continued research and innovation will likely result in future monitors that are more accurate, user-friendly, and accessible. New capabilities could help address existing limitations and accommodate a variety of needs.
