Posted July 17, 2025 in Fertility Blog & Information
15 minute read
Key Takeaways
- A balanced endometrial microbiome facilitates immune modulation, gene expression, metabolism, and protection against bacterial infections that negatively affect reproductive health.
- Dysbiosis can cause fertility issues, implantation failure, endometriosis, or chronic endometritis.
- Precise diagnostics, such as meticulous sample collection and sophisticated analysis methods, are key for detecting microbial patterns and informing therapy.
- Adding probiotics and lifestyle medicine and targeted antibiotic therapies can help restore and maintain a healthy endometrial microbiome.
- Interactions between the endometrial, vaginal, and gut microbiomes highlight the importance of systemic health and an integrated approach to reproductive wellness.
- By tracking and nurturing a rich community of helpful microbes, we could enhance reproductive success and promote fertility for people everywhere.
Endometrial receptivity microbiome means the mix of bacteria and other microbes that live inside the lining of the uterus when it is ready for an embryo to attach. Studies show that the right balance of these microbes can play a key role in fertility and healthy pregnancy outcomes. A healthy endometrial microbiome often means more Lactobacillus species, which links to better chances of a successful embryo implant. Imbalances, like too many harmful bacteria, may lower the odds of getting pregnant or increase risks in early pregnancy. Current research looks at ways to test and change the uterine microbiome to help people facing infertility. The next parts of this blog post will cover how the microbiome works, how to test it, and possible treatment choices.
Microbiome’s Influence
This endometrial microbiome molds the receptivity of the uterus. Research connects its composition to the likelihood of embryo implantation, particularly in assisted reproduction. Endometrial microbiome is usually Lactobacillus dominant, around 80-90% or more. This balance prepares the endometrial lining to support the embryo and increases the likelihood of a successful pregnancy. The microbiome shifts with age, hormone changes and even contraceptive devices, which can increase risks of things such as chronic endometritis and recurrent implantation failure. Diversity decreases with age and younger women’s microbiomes are more similar.
1. Immune Modulation
The endometrial microbiome communicates with the immune system, modulating the body’s response at implantation. Lactobacillus spp. Keep inflammation low and help the immunity not attack the embryo. They allow the body to develop tolerance as a new embryo comes in, reducing the likelihood of immune rejection. When this system works, the uterus welcomes the embryo, supporting pregnancy. If the balance tips, chronic inflammation or infections, such as endometritis, can ensue, increasing the risk of implantation failure.
2. Gene Expression
Different types and concentrations of bacteria in the uterus can modify which genes are activated or suppressed in the endometrial lining. Others microbial byproducts tweak the DNA signals instructing the cells to prepare for implantation. For instance, Lactobacillus can aid in switching on genes that facilitate embryo attachment, whereas pathogenic microbes could have the opposite effect. Immune, cell adhesion and nutrient supply genes all rely on these microbial cues. Gene expression changes from a dysbiotic microbiome can reduce the probability of a healthy pregnancy.
Microbial metabolites—short chain fatty acids, for instance—serve as messengers, direct gene expression. This implies that what’s growing in the womb could literally direct the entire process of embryo rejection.
3. Metabolic Function
A good microbiome in the endometrium produces helpful substances, such as vitamins and fatty acids, that nourish the uterine lining. These nutrients assist the lining to become thick and prepared for an embryo. Friendly bacteria maintain the pH stable and inhibit the growth of pathogenic bugs. Without them, the endometrium may not be supportive enough and embryo development decelerates.
Others degrade hormones and maintain balance. This is crucial for a healthy period and for the window when the uterus is most receptive to pregnancy.
4. Pathogen Defense
The microbiome can prevent harmful bacteria from dominating the uterus. Good bacteria such as Lactobacillus produce acids and antimicrobial agents that inhibit pathogens. If this defense wanes, infections — such as bacterial vaginosis or endometritis — can take hold.
Infections damage fertility. They trigger inflammation and can be damaging to the embryo. Rebalancing the microbiome with antibiotics or probiotics can assist. However, outcomes differ.
When good bugs triumph, the womb is more secure for fetuses.
5. Embryo Signaling
Endometrium bacteria even assist in sending signals that instruct the lining on when to permit an embryo to implant. Microbial byproducts assist the embryo and uterus to ‘communicate’ so that implantation occurs at the appropriate time. If the microbiome is out of whack, these signals can become mis-communicated, and pregnancy may not begin.
If we can target the microbiome with tailored treatments, we may be able to repair signaling problems and increase implantation success rate.
Microbial Profiles
A good endometrial microbial profile is one in which most of the bacteria belong to the genus Lactobacillus. These bacteria maintain homeostasis by acidifying the pH and preventing the colonization of pathogenic organisms. Scientists typically refer to a profile as being “Lactobacillus-dominant” when these microbes account for 90% or more of the population. For controls, median relative abundance of Lactobacillus can be 81% up to almost 98%. For RIF patients, levels fall but still represent a high percentage, approximately 92%. Infertile patients with a non-Lactobacillus-dominant (NLD) profile have less Lactobacillus and more of others, such as Prevotella, Gardnerella and Ralstonia. These diversity changes are associated with worse reproductive outcomes. The following table compares microbial diversity in fertile and infertile individuals:
| Group | Lactobacillus (%) | Prevotella (%) | Gardnerella (%) | Ralstonia (%) |
|---|---|---|---|---|
| Control (Fertile) | 97.96 | Least abundant | Not enriched | Not enriched |
| RIF (Infertile) | 92.27 | 2.19 | 2.18 | 1.15 |
Certain microbial strains, particularly Lactobacillus, correlate with increased implantation and pregnancy success rates. Tracking these profiles provided distinct indicators of reproductive health and aided clinical evaluation.
Favorable Bacteria
- Lactobacillus crispatus
- Lactobacillus iners
- Lactobacillus jensenii
- Lactobacillus gasseri
These bacteria maintain the endometrial environment in equilibrium by producing lactic acid, which lowers pH and inhibits colonization of undesirable organisms. A diverse blend of these good bacteria is associated with an increased likelihood of conception and decreased risk of infections. Maintaining a diverse population of beneficial bacteria balances the immune response and contributes to healthy tissue.
Consuming a nutritious diet, administering probiotics, and not taking excessive antibiotics may all help stimulate the growth of good bacteria in endometrium.
Unfavorable Bacteria
Gardnerella vaginalis, Prevotella spp., and Ralstonia spp. are often found in higher amounts in patients with RIF or other fertility problems.
Elevated levels of these bacteria can disrupt the endometrial environment. This, in turn, may cause inflammation, unhealthy tissue and a decrease in implantation potential.
Dysbiosis, or a loss of microbial balance, increases the risk of pregnancy complications. Women with more of these bacteria tend to have higher rates of miscarriage or failed implantation.
Targeted antibiotic or probiotic use can reduce these undesirable bacteria and rebalance the microbes.
Monitoring and Assessment
Microbial profiles as markers in reproductive checkups
Simple to test and able to inform treatments for improved results.
Physicians would be able to detect changes in microbe populations early and head off problems.
Dysbiosis Consequences
Dysbiosis in the endometrial microbiome refers to an imbalance of bacteria. This can impact fertility, pregnancy, and even long-term reproductive health. Endometrial microbiome contributes to a healthy environment for embryo implantation and growth. Dysbiosis is typically characterized by lower amounts of Lactobacillus and an elevation of other bacteria. Signs and symptoms may include:
- Irregular menstrual cycles or abnormal bleeding patterns.
- Chronic pelvic pain or discomfort.
- Difficulty conceiving or repeated implantation failure.
- History of recurrent miscarriage.
- Increased pelvic infections or inflammation.
- Unexplained infertility despite normal test results.
Implantation Failure
Dysbiosis is often linked to higher rates of failed implantation in fertility treatments. Reduced Lactobacillus and the rise of bacteria like Gardnerella vaginalis or Streptococcus can trigger inflammation, making it harder for an embryo to attach. Studies show that lower anti-inflammatory markers, such as IL-10, and higher inflammatory molecules are common in these cases, which further disrupts the uterine lining.
Specific microbial profiles — like non-Lactobacillus dominance or elevated Ureaplasma — are associated with negative outcomes. In others, re-establishment of a healthy Lactobacillus-dominant environment with targeted antibiotics or probiotics has enhanced implantation. Case studies from fertility clinics identify women who, once their microbiome was restored, were able to get pregnant after trying for years unsuccessfully.
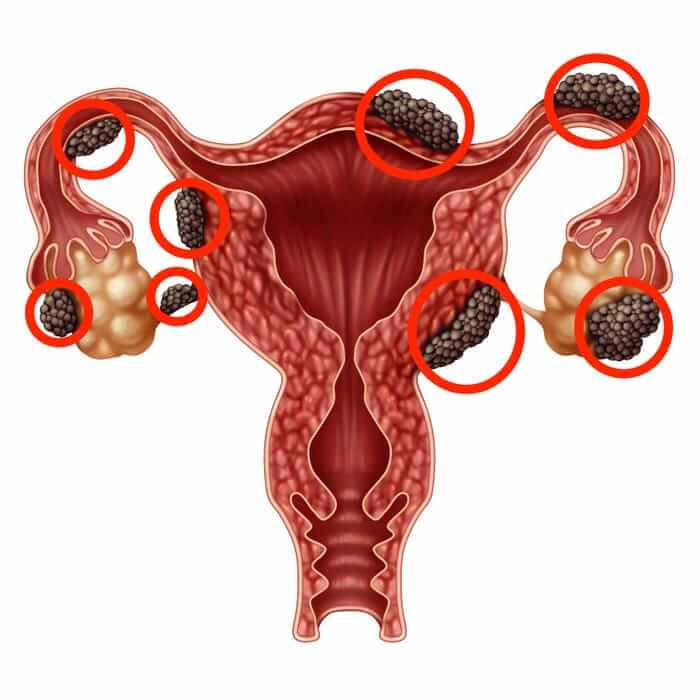
Endometriosis Link
Research shows a close link between endometrial microbiome dysbiosis and endometriosis. Women with endometriosis often have less bacterial diversity, with a higher presence of Atopobium vaginae, Prevotella bivia, and Bifidobacterium. These changes may worsen endometriosis symptoms by encouraging inflammation and tissue growth outside the uterus.
Treatments oriented towards shifting the microbiome, be it through targeted antibiotics or probiotics, are being investigated. When discovered and treated early, it can slow endometriosis progression, providing hope for symptom relief and improved fertility.
Chronic Endometritis
Chronic endometritis is persistent inflammation of the endometrial lining and is frequently associated with microbiome imbalances. Bacteria like Gardnerella or Ureaplasma can perpetuate infection, reducing Lactobacilli and increasing inflammation. This can damage fertility.
Treatment involves antibiotics and occasionally probiotics to restore a healthy equilibrium. Whether or not you have CE, treating this infection can increase your odds of having a healthy pregnancy.
Diagnostic Methods
Evaluating the endometrial microbiome depends on accurate diagnostics to uncover microbial communities associated with endometrial receptivity. Trustworthy results require thorough sampling, strong analysis, and standardized protocols—each essential for associating microbiota with fertility.
Sample Collection
Endometrial specimens are optimally obtained through sterile instruments, commonly in the proliferative or secretory phase, to identify pertinent microbial changes. The technique is important — endometrial biopsies, aspiration or sampling from the distal tip of an embryo transfer catheter are popular. Timing complicates analysis because microbial profiles may vary throughout the cycle.
Contamination is a major concern. Even slight introduction of vaginal or cervical microbes can skew results. Using sterile techniques, avoiding contact with non-endometrial surfaces, and minimizing handling helps. Samples should be placed in sterile containers and kept cool for transport, as microbial DNA degrades with heat and time.
Analysis Techniques
| Method | Advantages | Limitations |
|---|---|---|
| Culture-based | Identifies viable bacteria | Misses non-culturable species |
| 16S rRNA gene NGS (e.g., Ion Torrent) | Broad coverage, high sensitivity | May detect contaminants |
| Pyrosequencing | Detects mixed DNA, high throughput | Expensive, requires expertise |
| PCR amplification (30 cycles, 10 µL) | Sensitive for low-biomass samples | Prone to contamination |
Culture-based methods reveal what grows, but overlook most bacteria. Molecular methods, such as 16S rRNA gene sequencing, can identify both abundant and rare microbes. Pyrosequencing of cloned amplicons will help detect mixed bacterial DNA, indicating contamination. Emerging technologies such as real-time PCR and quantitative platforms like MultiskanGO enable detection and quantification.
Quality data is key. Most employ a 95% confidence interval with Student’s t distribution to define reference ranges for bacterial taxa. This aids in connecting microbial profiles to reproductive results, though variation in technique or sample handling can impact findings.
Standardization Needs
There are different protocols between labs and even between studies, making results difficult to compare. Standardizing collection timing and handling, DNA extraction, and sequencing methods can build trust in findings. Reference ranges, like those constructed using 95% confidence intervals, back standardized interpretation.
Therapeutic Potential
Studies of the endometrial receptivity microbiome have pointed to a few exciting directions. They span from probiotics and antibiotics to lifestyle and even stem cell-based therapies.
Probiotics
Certain probiotic strains, such as Lactobacillus crispatus and Lactobacillus jensenii, are commonly linked to a balanced endometrial microbiome. These bacteria can help keep harmful microbes in check and support a healthy environment for embryo implantation. Probiotics work by making the vaginal and endometrial pH more acidic, which limits the growth of pathogens. They help modulate immune responses and reduce inflammation, both important for fertility. Clinical studies have shown that women taking probiotics with these strains may see improved chances of conception and reduced recurrence of infections. To add probiotics safely to a reproductive health plan, focus on strains with strong clinical backing, avoid products with unclear labeling, and check with a healthcare provider first.
- Do: Choose clinically studied strains, follow recommended doses, consult a specialist before starting, and use products with clear labeling.
- Don’t: Self-prescribe without guidance, assume all probiotics are equal, or use them as a substitute for prescribed therapies.
Antibiotics
Antibiotics can be effective in treating dysbiosis of the endometrium microbiome and might increase fertility if an infection exists. Broad-spectrum antibiotics can damage helpful bacteria, potentially exacerbating the dysbiosis. Overusing antibiotics can cause resistance and risk of recurrent infections. Targeted antibiotic therapy– i.e., based on culture results — minimizes these risks by addressing specific pathogens. Options such as probiotics, lifestyle changes, or even stem cell-derived exosomes could assist in bringing back balance without the down-side of antibiotics.
Lifestyle Impact
A balanced diet, consistent exercise, and stress reduction can all contribute to the endometrial microbiome. By nourishing the good bugs with fiber-rich, fermented foods, and lean protein. Both regular movement – which increases circulation and immune health – and stress reduction – which helps reduce inflammation – are critical. A holistic approach, which may encompass sleep hygiene and mindfulness, can additionally refine reproductive outcomes.
- Eat a diverse, fiber-rich diet with fermented foods.
- Move daily with moderate-intensity exercise.
- Manage stress using mindfulness or relaxation techniques.
- Prioritize sleep and limit processed foods.
Systemic Crosstalk
Systemic crosstalk refers to the communication between various body systems, such as the gut, uterus, and hormones. These connections are important for reproductive health, particularly regarding the endometrial microbiome. How these systems signal through hormones, neurotransmitters and other molecules can influence fertility and pregnancy outcomes. Knowing these connections illuminates why a wide-lens, full-body perspective is essential for reproductive health.
Vaginal Connection
The vaginal microbiome and endometrial health are closely linked. A balance of bacteria, mainly Lactobacillus, in the vagina can help shape the environment of the upper reproductive tract, including the endometrium. When the vaginal flora is out of balance, it can let harmful bacteria move upwards, which may affect implantation or raise the risk of infection.
Keeping the vaginal microbiome healthy is key for overall reproductive wellness. Regular hygiene, safe sex practices, and avoiding harsh soaps or douches help keep the natural flora in check. Some studies suggest probiotics or prebiotics as ways to support healthy vaginal bacteria, but more research is needed before making broad recommendations.
Gut-Uterus Axis
The gut-uterus axis demonstrates how gut bacteria can modify endometrial function. Microbe-produced short-chain fatty acids (SCFAs) such as acetate and butyrate can be involved in hormone release and immune responses in the uterus. For instance, supplementing mothers with short- and medium-chain fatty acids has exhibited enhanced pregnancy rates and embryo implantation in certain studies, rendering diet an actionable lever.
A healthy gut lays the foundation for optimizing fertility. Consuming a lot of fiber and fermented and plant-based foods nourishes the gut microbiome. All of these foods help maintain SCFAs at good levels, which can help support a receptive endometrial lining.
Dysfunctions in this system, as seen in polycystic ovary syndrome (PCOS) or recurrent implantation failure, demonstrate just how crucial gut health is to reproductive success.
Hormonal Interplay
Hormones and the microbiome influence one another in a feedback cycle. Hormonal fluctuations, such as those during a menstrual cycle, can alter which microbes flourish in the reproductive tract. In turn, the microbiome can impact hormonal function, with hormones like estrogen, leptin, and insulin having downstream impacts on endometrial receptivity.
Hormonal and microbiome balancing therapies—targeted probiotics, diet shifts, hormonal treatments—may assist those facing fertility issues. These techniques help to establish a more secure setting for embryo implantation and development.
Toward Integrated Health
Whole-body approaches are needed in reproductive health. Sustainable health is found in viewing the body as an ecosystem. Every system counts in fertility. Care is best when it’s comprehensive.
Conclusion
Healthy balance in the endometrial microbiome contributes to how the uterus accepts and sustains an embryo. Changes in these minuscule organisms can lead to actual alterations in fertility and embryo development. Doctors now have new tests to examine these alterations. Some clinics attempt to correct imbalances with probiotics or other measures. All of these steps are promising, but additional research can indicate which treatments work best. Obvious connections connect the microbiome to the entire body, not merely local regions. Supported by real trials and solid evidence, this area is expanding. Those interested in hearing more or speaking with a care team can begin by inquiring about the new insights in endometrial health and microbiome care.
Frequently Asked Questions
What is the role of the microbiome in endometrial receptivity?
The microbiome assists in forming a balanced uterine environment. This equilibrium fosters embryo implantation and healthy pregnancies by mitigating inflammation and enhancing optimal endometrial function.
Which microbes are commonly found in a healthy endometrial microbiome?
A Lactobacillus-dominated endometrial microbiome is indicative of a healthy endometrial receptivity. These bacteria support a steady and protective environment for the endometrium.
How does dysbiosis affect fertility?
Dysbiosis, an imbalance in the microbiome, can increase inflammation and inhibit endometrial receptivity. This can decrease the likelihood of viable implantation and pregnancy.
What are common methods to diagnose endometrial microbiome issues?
Doctors may utilize molecular methods such as PCR and next-generation sequencing to detect and characterize the endometrial microbiome.
Can the endometrial microbiome be improved through treatment?
Indeed, targeted treatments like probiotics or antibiotics could potentially heal a microbial imbalance. This may enhance endometrial receptivity and thus the ability to conceive a pregnancy.
How does the endometrial microbiome interact with other body systems?
The endometrial microbiome can impact and be impacted by the gut microbiome and immune system. This systemic crosstalk may influence overall reproductive health.
Why is it important to study the endometrial microbiome globally?
Knowledge of the endometrial microbiome in various populations aids in refining diagnostics and therapeutics. It makes sure care is impactful and accessible for individuals everywhere.
